Abstract
Downmodulation of antigen presentation machinery represents a paradigm of evasion from adaptive immune surveillance. This mechanism underpins the decrease in presentation of immunogenic peptides below the activation threshold of effector T-cells. Large genomic aberrations, fine somatic mutations, epigenetic silencing and transcriptional modifications involving directly the human leukocyte antigen (HLA) region or genes encompassing antigen degradation, transportation and processing have been invoked across large cohorts of solid tumors and hematological disorders, all as a result of a common lynchpin: the established immune pressure. During tumor growth this orchestra of mechanisms shape the oncogenic landscape and facilitate the emergence of clones with lower immunogenic potential.
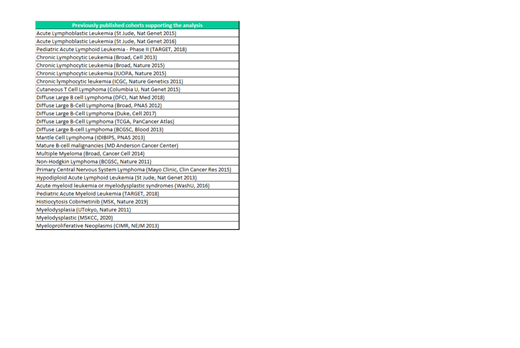
By analyzing genomic profiles extracted from more than 7000 patients and specimens across 25 previously published cohorts encompassing both lymphoid and myeloid diseases (Table 1), we performed a large genomic study aiming to dissect the multifaceted immunoediting processes in hematological malignancies
We first analyzed a broad HLA genomic dysfunction in 31 classical and non-classical loci and identified 892 somatic mutations or allelic losses in 337/6694 patients (5%). Among the different subtypes of hematological malignancies, HLA mutations were found in 16% (N=138/831) of acute lymphoblastic leukemia (ALL), 7% (N=1/14) of histiocytic disorders, 7% (N=3/43) of T-cell lymphoma, 6% (N=136/2247) of myeloid disorders, 2% (N=4/205) of multiple myeloma, 1.6% (N=55/3354) of B-cell lymphoma/chronic lymphocytic leukemia (B-LNH/CLL). Most affected loci were classical A, B and DRB1, while non-classical DPB2, F and DOA were the least interested by somatic events. Interestingly, alterations were never found in non-expressed DRB genes (DRB2-4,7-9). Among the immune genes, we focused on those which, if affected by mutations (either loss or gain of function), could possibly be associated with an immune escape signature. We identified such aberrations in 13% of cases, including CREBBP (4.5%, N=450/9875), EP300 (2.5%, N=252/9831), IRF8 (2.1%, N=166/7865), B2M (2%, N=158/7868), CD70 (1.7%, N=127/7253), TNFRSF14 (2.8%, N=221/7868), IRF4 (1.4%, N=110/7869), which were the most frequently altered. The frequency of those mutations was particularly high in B-NHL/CLL (28%) and ALL (23%). These events and HLA hits were not mutually exclusive. When analyzing the pattern of co-mutations in immune aberrant vs. non-aberrant group, we found that both lymphoid and myeloid entities were enriched in genomic abnormalities also in other immune players (e.g., NOTCH4, NFKB1, IL4R, IFNAR2, C3), emphasizing how the genomic dysfunction of the immune response may be a pathophysiological link, beyond the disease ontogenic classification. Of note is that, in MN subset, aberrations in leukemic drivers, such as: NPM1 (3% vs 16%, q=4.69E-11), JAK2 (3% vs 9%, q=1.00E-04), FLT3 (7% vs 14%, q=1.26E-04), SRSF2 (4% vs 10%, q-value=2.20E-04), DNMT3A (13% vs 21%, q=.001), TP53 (6% vs 10%, q=.009), NRAS (7% vs 12%, q=.021) were enriched in the non-immune-altered group. When accounting for the total number of mutational events, we found that this was significantly increased in immune aberrant vs. non-aberrant cases (q-value=10e-10) in both lymphoid and myeloid disorders. These findings are consistent with the hypothesis that HLA and immune defective escaping clones may arise in the context of a strong anti-tumor response, as a negative feedback to the immunoediting responsible for sculpting the tumor clonal burden. While driver hits can easily gain a fitness advantage regardless of the acquisition of immune escape signatures, immune-aberrant clones (especially if lacking more strong leukemogenic hits) would accrue subclonal alterations as a result of evasion from tumor surveillance, promoting growth only when opposing immune response.
In analogy with solid cancers, our results show that also in hematological malignancies, the biology underpinning immune escape mechanisms is intimately related to the processes of immunoediting and may shape malignant clonal progression. In this setting, mutations in determinants of immune responsiveness might constitute markers of operative tumor surveillance.
Maciejewski: Novartis: Consultancy; Bristol Myers Squibb/Celgene: Consultancy; Regeneron: Consultancy; Alexion: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal